
AC Joint Injuries in Hockey: Types, Symptoms, Treatment & Rehab Protocol
What Is an AC Joint Injury (Shoulder Separation)?
An acromioclavicular (AC) joint injury – often called a shoulder separation – is an injury to the joint at the top of the shoulder where the collarbone (clavicle) meets the shoulder blade’s acromion . Unlike a shoulder dislocation (which involves the ball-and-socket joint), an AC joint injury involves tearing or spraining of the ligaments that hold the clavicle and acromion together. This results in the clavicle separating from the acromion to varying degrees, hence the term “shoulder separation.” In hockey players, AC joint injuries commonly occur from a hard fall onto the shoulder or a direct blow – for example, a check into the boards or a collision on the ice that drives the shoulder downwards .
Why are AC joint injuries so common in hockey? Hockey is a high-impact sport with frequent collisions and falls at high speed on hard ice. AC joint injuries are the most common upper extremity injury in ice hockey players , largely because players often experience heavy contact that drives the shoulder into the ice or boards. When the shoulder takes a forceful impact (especially with the arm adducted against the body), the AC ligaments can be sprained or torn, leading to separation of the joint . Additionally, hockey players are typically young and active (often males under 35), which is the demographic most prone to AC separations in contact sports .
Types and Severity of AC Joint Injuries (Grades I–VI)
AC joint separations are classified by severity into Grade I through Grade VI (1–6), commonly known as the Rockwood classification . Higher grades indicate more severe ligament damage and greater separation of the joint. The classification helps guide treatment decisions . Grade I–III are considered mild to moderate (often managed without surgery), while Grade IV–VI are severe injuries that typically require surgical intervention .
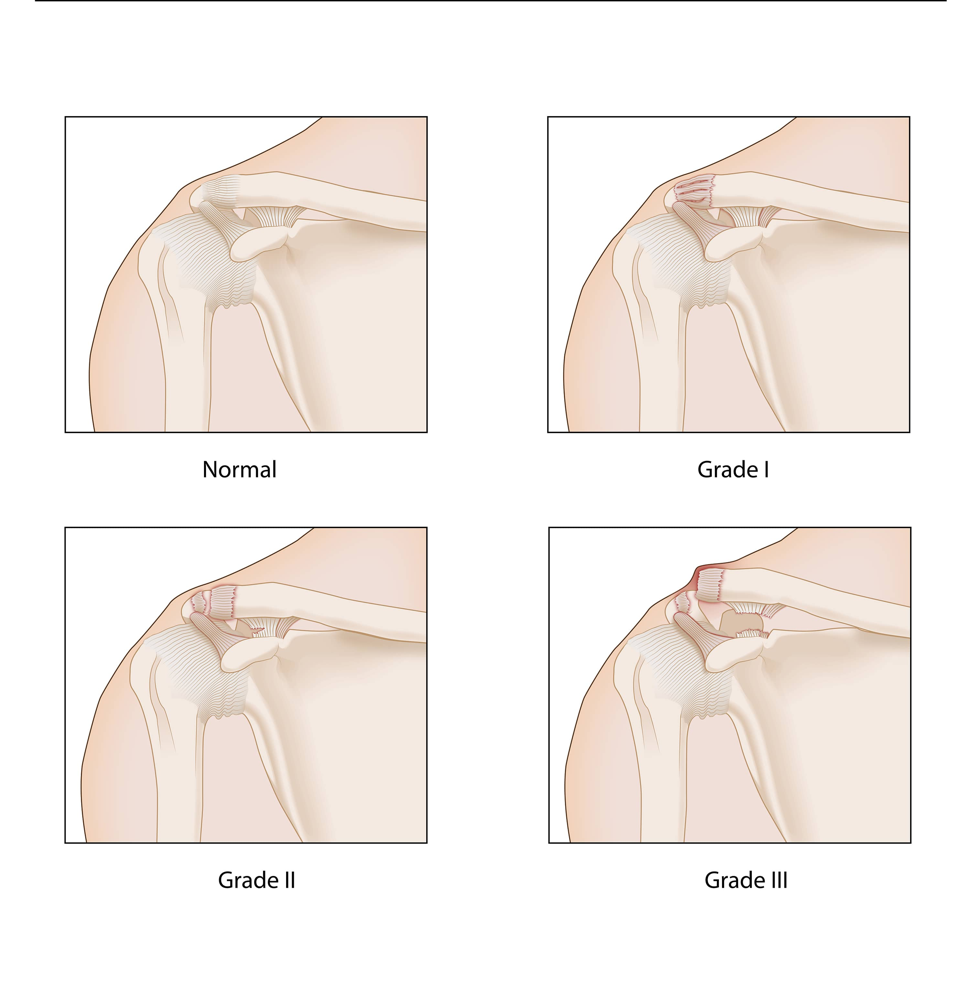
Illustration of AC joint separation severity (Normal vs. Grade I, II, III). In higher-grade separations, the end of the clavicle displaces upward, creating a visible bump on top of the shoulder. Each grade of AC joint injury can be described as follows:
- Grade I (Mild Sprain): The AC ligaments are stretched or mildly sprained but not torn. The clavicle remains in place. There is no visible deformity and the joint looks normal on X-ray . Symptoms are mainly pain and tenderness at the AC joint, but the joint is stable.
- Grade II (Moderate Sprain): The AC ligament is torn, and the coracoclavicular (CC) ligaments (which also stabilize this joint) are sprained or partially torn. This may cause a slight separation – the clavicle is out of alignment slightly, resulting in a small bump on the shoulder . The shoulder may have some horizontal instability, but the separation is usually less than 25% of the normal distance .
- Grade III (Complete Separation): Both the AC and CC ligaments are completely torn, causing a obvious separation. The clavicle is no longer held to the acromion, so it rides up, creating a noticeable bump at the AC joint. On X-ray, the distance between clavicle and coracoid (CC distance) can increase 25–100% compared to the normal side . The shoulder may look deformed or “step off” at the top. Despite the prominent bump, a Grade III injury can still often be treated without surgery in many cases .
- Grade IV (Posterior Displacement): A severe injury where the clavicle is pushed backwards into or through the trapezius muscle . All supporting ligaments are torn. This causes a significant deformity (with a prominent bump or posterior fullness on exam) . Grade IV injuries are not common and usually require surgical repair .
- Grade V (Severe Upward Displacement): An extreme version of a Grade III. The clavicle is severely elevated (often more than 100% higher than its normal position relative to the shoulder blade) . The shoulder droops downward markedly under the weight of the arm (since the “strut” support of the clavicle is gone) . This injury causes a very large bump and is usually not reducible without surgery, so operative treatment is typically recommended .
- Grade VI (Inferior Dislocation – Very Rare): An extremely rare injury where the end of the clavicle is displaced downward, underneath the coracoid or acromion (toward the ribcage) . It results from high-force trauma (such as a high-speed collision) and is often accompanied by other injuries . Grade VI also involves complete ligament disruption and requires surgery to relocate and fix the clavicle .
Most hockey-related AC joint injuries are Grades I–III (the milder end), but higher grades can occur with especially forceful impacts. Even a Grade I or II AC sprain can be very painful and temporarily debilitating, though these lower-grade injuries heal fairly quickly with proper care .
Symptoms and Diagnosis of an AC Joint Separation
Symptoms: An AC joint injury typically causes immediate pain on top of the shoulder at the moment of injury. Players often report sharp pain at the AC joint area, which may radiate into the neck or trapezius region . Soon after, the top of the shoulder can become swollen and tender to touch. Bruising may appear over the joint in the days following. In higher-grade separations, a visible bump or prominence appears at the AC joint – this is the end of the clavicle that has risen up. The injured athlete will have difficulty lifting the arm, especially overhead or across the body. Movements like reaching the arm across the chest (for example, to put on a seatbelt or throw a check in hockey) typically increase the pain. They might also feel that the shoulder is weak or “giving way” with certain motions due to the instability.
On physical exam, there is point tenderness over the AC joint and sometimes an obvious deformity (an “abnormal contour” at the shoulder) compared to the uninjured side . Pressing down on the clavicle may accentuate its movement like a piano key in higher grades. Pain is often reproduced with specific tests, such as the cross-body adduction test (where the patient brings the arm across the chest, compressing the AC joint) – this maneuver typically causes AC joint pain if injured . Shoulder range of motion is limited by pain, particularly when lifting the arm up or doing pushing motions.
Diagnosis: Doctors diagnose an AC joint separation through history, exam, and imaging. The mechanism of injury (fall on shoulder or direct blow in hockey) combined with the focal pain and any deformity strongly suggest an AC injury. Standard X-rays of the shoulder confirm the diagnosis and help determine the injury grade by measuring the separation . X-rays are usually done from the front (AP view) comparing both shoulders, and sometimes a special axillary lateral view is taken to detect any backward displacement of the clavicle (important for diagnosing a Grade IV) . In subtle cases (e.g. to distinguish Grade II vs III), some doctors may use stress views (holding a weight) to see if the joint widens, though this is less common today .
Occasionally, an MRI may be ordered for a severe injury or if the diagnosis is unclear. MRI can visualize the ligament damage and any additional injuries (like rotator cuff or cartilage injuries) in the shoulder . However, MRI is usually not required for routine cases. The combination of physical exam and X-ray is sufficient in most instances to classify the AC joint injury.
AC Joint Separation Treatment and Recovery Timeline
Initial treatment of an AC joint injury focuses on pain control and supporting the shoulder. Right after the injury, the player should ice the shoulder and may use a sling to support the arm and reduce stress on the AC joint. Rest and anti-inflammatory medications (e.g. ibuprofen) help reduce pain and swelling . For very mild injuries (Grade I), a sling might only be needed for a few days until pain subsides. For Grade II or III injuries, a sling is often worn for 1–2 weeks or slightly longer to allow the torn ligaments to begin healing . During this period, one should avoid heavy lifting or movements that aggravate the shoulder.
Whether or not surgery is needed depends on the severity (grade) of the separation and the athlete’s needs. The general approach to AC joint separation treatment is:
- Non-Surgical (Conservative) Treatment: This is the first-line for most Grade I, II, and even many Grade III injuries . Conservative management includes immobilization in a sling briefly, ice, rest, and early physical therapy to restore motion and strength . Most AC joint injuries in recreational and even professional hockey players are treated without surgery unless there is gross deformity or persistent instability. Research shows that even high-grade (Grade III) separations often heal well without surgery, with outcomes comparable to surgery if rehab is done properly . By avoiding surgery, athletes eliminate surgical risks and can often return to sport sooner. For example, many NHL players with Grade I–III AC separations return to play in as little as 2–4 weeks once pain allows , wearing protective padding. In non-elite athletes, return might be closer to 6–12 weeks to regain full strength . Rehabilitation is critical during non-operative treatment – we’ll discuss the rehab protocol in the next section.
- Surgical Treatment: Surgery is generally reserved for severe separations – typically Grades IV, V, and VI, or certain Grade III cases (for instance, in elite athletes or if the clavicle is profoundly displaced and unstable) . In these injuries, the clavicle is significantly out of place and the torn ligaments won’t heal back adequately on their own. Surgical techniques involve restoring the normal alignment of the clavicle and acromion (called reduction) and fixing them in place with hardware or by reconstructing the torn ligaments. There are various procedures (such as using a screw, suture anchors, or graft to rebuild the coracoclavicular ligaments). The goal is to stabilize the joint so the ligaments can heal in the correct position . After surgery, the arm is kept in a sling for several weeks to protect the repair . Physical therapy is still required after surgical repair, but starts later and progresses more cautiously than in non-operative cases. The overall recovery timeline with surgery is longer – often about 4 to 6 months before return to full sport activities – because it takes time for the reconstructed ligaments to heal and for strength to return. Surgery can successfully restore stability and has a high rate of return-to-sport in athletes , but it also carries risks like any surgery (infection, hardware problems, or persistent pain in some cases).
Recovery timelines vary with the injury grade and treatment route. For a Grade I AC sprain, a hockey player might be back on the ice in 1–2 weeks, as pain allows, using shoulder protection. Grade II injuries often heal in about 3–4 weeks, and a return to play by 4–6 weeks is common with rehab. Grade III injuries (non-surgical) typically require around 6–12 weeks of rehabilitation for full return to high-level play , though some pros accelerate this. If a Grade III is treated surgically (which might be chosen for certain competitive athletes), it then follows the longer surgical timeline (several months). Grades IV–VI, which nearly always need surgery, will sideline an athlete for several months; usually the player can resume full training around the 5–6 month mark post-op, once cleared by the surgeon .
It’s important to note that every athlete’s recovery can differ. Pain levels and healing rates vary. A key milestone for returning to hockey (or any sport) after an AC joint separation is regaining full, pain-free range of motion and near-normal shoulder strength. Players must also be able to perform sport-specific tasks (for hockey, that includes shooting, checking, stick-handling) without limitation. A proper rehabilitation program is essential to meet these goals, whether managing the injury conservatively or post-surgery . In the next section, we’ll explore an advanced AC joint rehab protocol designed for athletes, like the one used at Ghost Rehab, to optimize recovery.
Ghost Rehab’s Advanced AC Joint Rehab Protocol for Athletes
Rehabilitation is the cornerstone of recovery from an AC joint injury. At Ghost Rehab – a sports physical therapy and performance clinic – our team takes an advanced, multi-modal approach to shoulder rehab for athletes. Our AC joint rehab protocol is evidence-based and tailored to the unique demands of hockey players and other athletes. Key components of Ghost Rehab’s rehab approach include:
- Dry Needling for Pain Relief: We incorporate trigger point dry needling to help alleviate muscular pain and guarding around the shoulder. Dry needling uses fine needles (similar to acupuncture needles) inserted into tight or knotted muscles to release tension and reduce pain. This can be especially helpful for AC joint injuries, where muscles like the trapezius and deltoid may become very tight or sore after the trauma. By relieving these myofascial trigger points, dry needling can improve shoulder mobility early in the rehab process and provide significant short-term pain relief . Reduced pain enables the athlete to perform exercises more effectively during therapy.
- Myofascial Release and Manual Therapy: Ghost Rehab’s clinicians are experts in manual therapy techniques to restore mobility. Myofascial release involves hands-on techniques to stretch and loosen the fascia and muscles around the shoulder. After an AC separation, it’s common to develop tightness in the chest, neck, and shoulder muscles as the body tries to protect the area. Gentle joint mobilizations and soft tissue release can improve range of motion and decrease stiffness . For example, mobilizing the scapula and clavicle can help normalize movement at the AC joint as it heals. These techniques not only address the AC joint itself but also the shoulder blade and spine, which must move properly for the shoulder to function. By improving tissue flexibility and breaking up adhesions, myofascial release helps the athlete regain full motion without pain.
- Neuromuscular Re-education: After the initial injury and immobilization phase, the shoulder may “forget” how to move in sync due to pain and disuse. Neuromuscular re-education is used to retrain proper movement patterns and muscle firing sequences. This means teaching the shoulder and shoulder blade (scapula) muscles to work together smoothly again. For instance, exercises focused on scapular stabilization (like gently pinching shoulder blades together) and proprioceptive drills help restore normal biomechanics. At Ghost Rehab, we utilize techniques like rhythmic stabilization, balance exercises, and sport-specific movement training to rebuild the brain-muscle connection. The goal is to regain normal, controlled movement patterns in the shoulder . Neuromuscular re-ed ensures that as strength returns, it does so with correct form – crucial for athletes who need efficient, safe motion on the ice. Poor movement patterns can lead to compensations or re-injury, so this step is vital for long-term success.
- Progressive Strengthening and Sport-Specific Rehab: Building back strength is essential, but it must be done progressively. Our therapists design an individualized strengthening program that starts with gentle exercises and advances over time as healing progresses. Early on, isometric exercises (where the muscles contract without moving the joint) may be used around the shoulder to maintain muscle engagement without straining the AC joint. As tolerated, we introduce resistance bands and light weights to strengthen the rotator cuff, deltoids, trapezius, and the muscles that support the shoulder blade. A balanced shoulder-strength program is crucial – we target not just the shoulder but also the upper back and core, since all these areas work together for healthy shoulder function . Over a few weeks, the rehab transitions into more challenging exercises: push-ups or chest press (modified as needed), overhead lifting exercises, and eventually plyometric or explosive movements that mimic hockey actions (such as medicine ball throws to simulate shooting). This graded exercise progression builds the shoulder’s tolerance and strength back to pre-injury levels. By the end of rehab, the athlete performs high-level activities – like shooting pucks, performing stick checks, and bracing for contact – under the guidance of the therapist. This ensures they are truly ready for the demands of competitive play.
Ghost Rehab’s comprehensive protocol not only treats the injury but also addresses any underlying weaknesses or movement issues to prevent future injuries. Throughout rehab, we emphasize proper technique and body mechanics. Each session is one-on-one, allowing close supervision and adjustments. Modalities like cold therapy or electric stimulation might be used adjunctively for pain or swelling as needed, but active rehabilitation is the centerpiece.
Expertise from a Former Pro Hockey Player and Doctor of Physical Therapy
One aspect that sets Ghost Rehab apart is the leadership and insight of our founder, Dr. Jamie Phillips. Dr. Phillips is a former professional hockey player turned Doctor of Physical Therapy . With over a decade of experience at the NCAA Division I and pro hockey levels, he understands firsthand the physical demands and mental pressures athletes face . This rare combination of high-level sports experience and clinical expertise means our athletes get care from someone who truly “speaks the language” of hockey and sports injuries.
Dr. Phillips has leveraged his on-ice experience to develop rehab strategies that are practical and sport-specific. He knows what it takes to get a hockey player back to game shape after an AC joint injury – not just healing the joint, but also maintaining conditioning, confidence, and hockey-specific skills. Under his guidance, Ghost Rehab blends cutting-edge therapy with personalized care to keep athletes performing at their best . Our team stays up-to-date on the latest sports medicine research and techniques, ensuring that treatments like dry needling and neuromuscular re-education are used effectively and safely. We also understand the importance of communication with coaches, trainers, and physicians during an athlete’s recovery.
In summary, Ghost Rehab provides shoulder rehab for athletes by athletes – combining sports-savvy care with evidence-based practice. For hockey players with AC joint separations, this means a quicker, safer return to the rink.
Conclusion: Recovery and Outlook
AC joint injuries in hockey are common but very treatable. With prompt diagnosis, appropriate management, and a structured rehab program, most players recover fully and return to their prior level of play. It’s crucial to allow the injured ligaments to heal while simultaneously rehabilitating the shoulder’s strength and mobility. Minor AC joint sprains may heal in a matter of weeks, whereas severe separations (or those requiring surgery) take several months – but even in the worst cases, athletes can often resume sports with no long-term limitation once recovered.
Key takeaways for players, parents, and coaches dealing with an AC joint separation: Rest the shoulder initially and don’t rush back too soon; follow a guided AC joint rehab protocol to rebuild strength and function; and consider seeking out sports rehabilitation experts (like Ghost Rehab) who understand the unique demands of hockey. With advanced techniques such as dry needling, myofascial release, and tailored strengthening, rehabilitation can be optimized for a faster recovery . The involvement of a skilled physical therapist can often mean avoiding surgery for moderate injuries and still achieving excellent stability and function .
Hockey is a tough sport, but injuries like AC joint separations don’t have to be career-threatening. With the right treatment plan and rehab team, a player can overcome a shoulder separation and get back to scoring goals or making big saves. In fact, many athletes come back feeling even stronger and more confident in their shoulders because of the comprehensive rehab process. The combination of clinical expertise and sports experience at Ghost Rehab ensures that every athlete has the best chance at a full recovery – and an educated understanding of their injury. If you or someone you know suffers an AC joint injury in hockey, remember that prompt care, proper rehab, and expert guidance are the keys to getting back in the game.
Optimizing Recovery, On and Off the Ice – AC joint injuries may be common in hockey, but with knowledge and the right approach, players can successfully return to the sport they love. Shoulder health is vital for shooting, checking, and every aspect of hockey performance, so taking an AC joint injury seriously and rehabbing it thoroughly will pay off in both the short and long term. Ghost Rehab’s team is here to help athletes navigate that journey from injury to full recovery, using a proven blend of advanced therapy techniques and firsthand sports insight to keep our hockey players at the top of their game.
References:
- Orthobullets – Acromioclavicular Joint Injury (Shoulder Separation) Overview .
- AOSSM Sports Medicine Update (Winter 2023) – Impact of AC Joint Injuries in Ice Hockey .
- OrthoInfo – AAOS: Shoulder Separation (AC Joint Injury) Patient Guide .
- OrthoInfo – AAOS: Shoulder Separation Treatment .
- Orthobullets – AC Joint Injury Classification and Treatment .
- Clinical Study – Return to Play After AC Joint Injuries in NHL Players .
- Dry Needling Research – Analgesic Effects in Shoulder Pain .
- Physical Therapy Guide – AC Joint Injury Rehab and Exercises .
- Ghost Rehab – Founder’s Profile (Dr. Jamie Phillips) .

.png)


